What to do if you are a patient or have a loved one in the Emergency Room
This post is dedicated to all the other nurse family members and friends out there.
As the emergency nurse in my family and friend circle, I am almost always one of the first calls or texts by people when they wind up in the ER or have a loved one that is an emergency patient.
First and foremost - I always tell the person on the other end of my call or text that I am so sorry that this is happening but please know that if you or your loved one is being taken to the emergency department, you most likely need to be seen by a medical provider and that the hospital is THE PLACE to be evaluated for all things medical. This often helps calm the person or at least put some of their concerns in perspective.
Next - I always validate whatever feelings they are having. It is normal to freak out when going to the ED or hearing that your loved one is going there. We do not have to be rational in a moment of crisis. Give people space to be emotional. Validate those feelings, then try to guide them back to the practical. I feel that is the greatest gift a nurse friend or family member can do - direct a person in crisis to something practical and addressing the scary unknown.
Now, if you’re reading this and you are not a nurse or medical person, WELCOME to the organized chaos that is emergency medicine! I am hoping this blog post will help clarify some of the confusion that you may be feeling and give support by answering some of the most common questions that I get as an emergency nurse friend and family member.
Clarification on the method to the madness that is emergency medicine:
Is it the ER or ED? Emergency Room vs. Emergency Department
Funny thing, it’s both. - The Emergency Department (ED) is the same thing as the Emergency Room (ER). You see, the specialty of emergency medicine was born in a room and originally, seemed confined to those original four walls. As the specialty became more advanced and comprehensive, we took up more than a room, and the ER went through a re-branding to become the emergency department. In common nomenclature and thanks to Hollywood, ER will always be more widely used. ED also stands for ‘erectile dysfunction’ in medicalese, so there is that challenge too.
What happens when I or my loved one arrives to the ED?
The short answer: lots of things. - Being a patient in the ED is like being a Nascar car that just arrived in the pit and is getting a quick turnover by the pit crew. Upon arrival, a patient will be quickly registered in the computer system - this means that their name, DOB, and other personal data will be put in the computer to create a digital chart that medical providers will use to document their care. This is not when they ask for your health insurance.
At the same time as registration, the patient will be taken one of two ways into the ED (assuming no one is ahead of them) >> to the triage room/area or directly to an ED exam room. In either case, the patient’s vital signs (i.e. heart rate, blood pressure, oxygen saturation, respiratory rate, temperature) will be taken and documented, lots of questions asked about their health history (things that have happened to them in the past medically), about their current issues that have brought them to the ED today (AKA “Why are you here today?”), current medications, and screening questions that they ask everyone related to domestic violence (“Do you feel safe where you live?) and suicidal thoughts (“Have you thought about ending your life, harming yourself, or others?”). Do not take these screening questions personally. They are often mandated by a regulatory body to be asked to everyone who can answer them.
In the time of COVID-19, ED’s are incredibly full of patients 24/7 so more realistically, you will be waiting in the waiting room for a very long period of time (think many hours) if you come by private vehicle (AKA your car) or a very long time on an EMS gurney if you come by ambulance. There is also the chance that if you come by ambulance, you will be re-directed to the waiting room too to wait. I am sorry. This is just the reality of emergency care at this time.
As these questions are being asked, orders may be placed for an EKG, blood labs, medications, IV placement, or imaging like X-rays, ultrasounds, or in some cases, CTs ( AKA Cat Scans - no cats involved). If this is the situation, you may be quickly poked or transported somewhere to have pictures taken of various body parts. This is good. You want answers and to get answers, tests need to be done. However the results of these tests may take anywhere from 45 minutes to hours to come back. A medical provider will review any abnormal results with you at a later time.
To complete many of these tests, you will need to be undressed to your birthday suit and placed in a hospital gown and socks with those rubber skids on the bottom. Please do not fight medical staff as they try to undress you. It is for medical reasons and not our entertainment that we need to get you naked. if you have cultural needs that need to be addressed like needing a specific gendered medical staff to assist you while undressing or religious garments that need to be maintained in a certain way, please let your medical staff know, and they will do their very best to make those accommodations while also meeting your medical needs as quickly as possible.
All of these events can happen concurrently which is often why the patient feels like the car getting handled by a pit crew. Lots of stickers may suddenly be attached to you with cords going all over the place. There may be pokes with needles or probes in various orifices. You may be asked to produce body fluid samples like urine or sputum while all this is happening. None of this is ideal or often comfortable, but know that we are asking you to do each task with the goal of getting you the care that you need rapidly and efficiently.
After the initial triage or intake process is completed for my loved one, does that mean I saw a MD/doctor/provider such as an NP or PA?
Maybe! But probably not. - Sometimes a physician or advanced care provider (NP/PA) will see you as soon as you arrive to the ED. Most often, it will take anywhere from a few minutes to several hours to see a physician during your visit. Average ED visits in the United States take anywhere from 4-8 hours, often longer in our current pandemic world.
If I am not immediately seen by a MD/provider as soon as I arrive, are things even happening those first few minutes to hours?? - Fear not! Lots of things will happen before the MD/provider physically sees you. Thanks to collaborative care and technology, many things will be ordered on you based on your “complaint” or reason why you are in the emergency department. Labs, scans/x-rays, medications, IVs, fluids and more are ordered “per protocol” or through “standing orders” and will be started as soon as you are seen (when applicable).
What if I get there and nothing happens? - This may happen too. If that is the case and you are waiting for an extended period of time in the waiting room, there is a reason. There is always a reason. However nothing is perfect and if you feel that you are there for a very big reason, check back in with the front desk. However if they say there are lots of sicker people who are waiting ahead of you, get comfortable and try to be patient as you wait your turn.
Why aren’t I being seen faster?
Who gets seen first in the ED - The order of who gets seen first is not based on when people get there. It is based on a combination of complaint or illness/injury severity, timing, and who shows up next. Remember that the ED has two entrances - the front entrance where triage and the waiting room is + the ambulance entrance which you cannot see from the waiting room. The waiting room may be empty but ambulances might not stop coming, so it may appear that the ED is not busy from the waiting room while all the rooms are actually full of patients with a line out the ambulance door in the back. Please be patient as we work to get you and your loved one taken care of.
Who can come into the ED to visit or accompany me or my loved one?
It all depends. - This is a hard one. During high COVID-19 surges, there are often NO VISITORS allowed in the ED. The only exceptions are an adult guardian for minors, possibly a care giver or guardian for memory (EX: dementia) or cognitively impaired or delayed patients, and end-of-life patients. When it is not a COVID-19 surge, the ED usually will limit visitors to one per patient. Please keep all minors home who don’t need to be there - siblings of a kiddo being seen for example. Encourage worried family members not to come to the ED in times of crisis. I always recommend making a point person for communication for the family or friends so that all info is filtered through one person. It can be a great tool to keep communication clear and concise.
What should I bring to the ED if I am going as a visitor or as a patient?
If you are the patient and not going by ambulance (AKA - you have time to think about what to bring and collect it all.) - Things to bring - A LIST OF YOUR CURRENT HOME MEDICATIONS or your actual pill bottles of current meds, your POLST or advance directive if you have a copy, ID card, health insurance card, credit card, your cell phone, CELL PHONE CHARGER (the longer the cord the better) with wall plug, a change of clothes, a book or something to read, a computer or tablet if you need it. We usually encourage people not to bring valuables unless they absolutely need it because things can go missing in the ED. I wish that wasn’t the case, but just know it happens. DO NOT BRING FOOD OR DRINK TO CONSUME unless you can wait until after you see the provider and are told by the nursing staff that you can eat.
Free advice - DO NOT EAT OR DRINK ONCE YOU ARE IN THE ED.
If you are the patient and are brought in an ambulance - You bring exactly what EMS or the firemen say you can bring. Do not hold up anything if medics are trying to get you in an ambulance. If you do have a minute, grab A LIST OF YOUR CURRENT HOME MEDICATIONS or your actual pill bottles of current meds, your POLST or advance directive if you have a copy, ID card, health insurance card, credit card, your cell phone, CELL PHONE CHARGER (the longer the cord the better) with wall plug.
If you are a visitor to someone who came by ambulance as a patient - Often the patient will not have time to grab anything at all, so you can try to collect things for them.
In this case, I recommend bringing the following for a loved one in the ED who is a patient: A LIST OF THEIR CURRENT HOME MEDICATIONS or their actual pill bottles of current meds, their POLST or advance directive if they have a copy, ID card, health insurance card, credit card, their cell phone, CELL PHONE CHARGER (the longer the cord the better) with wall plug, a change of clothes, a book or something to read, a computer or tablet if they need it. We usually encourage people not to bring valuables unless they absolutely need it because things can go missing in the ED. I wish that wasn’t the case, but just know it happens. DO NOT BRING FOOD OR DRINK TO CONSUME for them. Just don’t. No patient in the ED should eat until instructed to do so by their ED nurse.
As a visitor of a patient in the ED, you really just need stuff to occupy yourself, keep your devices charged (the longer the cords the better + the wall plug), and $$$ to buy stuff to feed YOURSELF (NOT THE PATIENT until the ED nurse says so), and a way to get home. If it is a COVID-19 surge, ED staff will most likely not let you in the building, and you will have the option of waiting in your car in the parking lot or somewhere near by.
If you are a visitor who is not let in the ED and has to wait outside for updates, make sure the ED staff has your correct phone number. And make sure that you have a correct phone number that you can call for updates. We really mean well in the ED and try to call with updates when we can, but you may want to call and get updates at regular intervals. Ask the ED staff what those regular intervals are. Results come back at expected times, so staff should be able to tell you when the next update in information will be. If they say don’t call back for an hour, listen to them. If you call back too often, you will not get any updates and further stress the already stressed out ED staff.
What will happen to me or my loved one in the ED?
In the majority of situations, you will either stay overnight in the hospital or get discharged home. - There are only two final options as a patient - you will stay or go.
Staying overnight in the hospital is called “being admitted to the hospital”. For an admission to occur, you will need to be seen by an “admitting doctor” which can be a hospitalist (think your main doctor for your hospital stay) or a specialist depending on your injury or illness. This doctor is different from the ED provider/MD. The admission doctor will see you after your initial ED work-up (all the tests done in the ED to determine if you need to stay overnight in the hospital or not) is completed. Whoever the admitting doctor is, they will have to evaluate you or the patient (your loved one) and write admission orders. This is done still in the emergency department. At that time, they will request an inpatient/admission bed for you. That bed will then need to be assigned. This bed is a bed NOT in the emergency department, but in a different part of the hospital where you will stay for the duration of your hospital stay. It can take hours to days at times (sorry - blame COVID-19) but usually hours to get this bed assigned. Then you will be transported to that assigned room via a ride in an ED gurney (bed with wheels) or a wheelchair. Then you will be assigned a new nurse and settled into your room for your continued hospital care!
Being discharged home from the ED means that you are not sick or injured badly enough to need to stay overnight in the hospital. Congratulations! You get to go home! What will happen next - the ED MD will come tell you about all your test results, give you verbal discharge instructions, and tell you to go home. But WAIT! You still have to wait for the PRINTED discharge instructions and the official discharge talk from your ED nurse before you actually physically go home. If you don’t get printed discharge instructions and any paper copies of prescriptions (or instructions that your prescriptions have been sent to your pharmacy), you are not ready to go home yet. The ED nurse does this with you. You usually hear about your follow-up care plan, recommended follow-up appointments (as applicable), and a review of any medications you need to continue at home + where to get them. Listen to all of this. It may be a very quick talk with the nurse. You will probably be in a rush and trying to figure out how to get home + a million other things, but this talk with the MD and the ED nurse are often your best chance to get your initial questions answered.
If you get discharged home, you should ask for a copy of all your test results and a disc with all your imaging on it. - Depending on the facility, they will be able to get this to you in the ED at the time of your visit. In some facilities, they will tell you to go online and find this information via an online patient portal. At other facilities, you will be instructed to make a request via the Medical Records department. Whatever the answer, fine, but make sure you ASK FOR A COPY BEFORE YOU GO. If you forget, it’s fine. It’s just often easiest to get this info at the time of discharge.
If you get discharged home, do not forget to ask for any valuables that may have been locked up during your stay. - You will know if this is applicable. In some cases as an ED patient, you will be stripped down to your birthday suit, all your belongings placed in a bag, and locked up in a locker. At the end of your visit, make sure to claim your valuables. This is often at Security or Registration (front desk).
Getting home from the Emergency Department - You will need to get home if you are discharged from the ED. There are a few options.
If you are able to walk and talk, you get to figure out how to get home. If you arrived by ambulance, an ambulance will not take you home. You should consider calling a friend or family member, use a ride share service (EX: Uber, Lyft), or have the ED call you a taxi (Note: you will have to pay for this).
If you cannot walk or need O2 or other assistance due to chronic health conditions or new illness/injury, a non-emergency ambulance can be arranged to get you home. However this is done under very specific situations for insurance to cover this. Please ask your nurse about this if you think you or your loved one qualifies.
If you are a visitor for a loved one in the ED who is being discharged, feel free to drive them home (if appropriate). One of the best things you can do for a patient in the ED is provide a ride home. Make sure that they get all their belongings and have their discharge instructions (paper copy) before you leave. It is usually best to drive up to the entrance for the shortest walk/wheelchair ride to the car. if you or your loved one needs assistance to the car, let the ED staff know. If someone is available, they will be happy to help! It may just take a little while as most ED’s are very, very busy at the moment.
I hope that helps! That definitely does not cover it all, but I think it hits the basics on how to navigate the confusing world that is the emergency department as a patient or visitor. Please know that every emergency department staff is doing their best every day, every shift, but we are under unprecedented (and I HATE that word) stress right now. It is feast or famine in the ED, meaning that it is either the busiest day of the millennia or it is deathly chill. You never know when that will change, so make sure you bring your PATIENCE when visiting us.
— Sarah @ New Thing Nurse
PS. A few additional tips for anyone coming to the emergency department that will make the ED staff much more likely to be in a better mood with you:
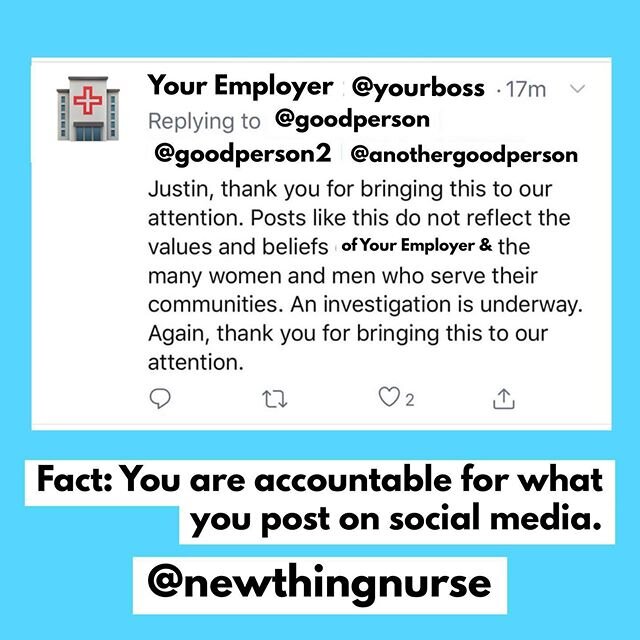
DO NOT yell, insult, harass, or even consider being violent with ED staff.
NEVER say that it is “qui*t” in the ED. - If there are not a lot of people in the ED, please never say that it is the “q-word”. It is bad luck. Just don’t say it. Also avoid using the word “sl+w”.
DO NOT EAT OR DRINK ONCE YOU ARE IN THE ED IF YOU ARE A PATIENT. Don’t eat on the way to the ED. Just don’t do it. And do not eat again until your ED NURSE says that it is ok. Not the ED MD, the ED Nurse. Just trust me on this.
If you are a visitor, do not ask the ED staff for food or beverages beyond water for yourself. There is usually a cafeteria. Or if you are allowed to leave and come back, feel free to go hit up vending machines or a close by drive-thru. We are here to care for your loved one, not you. No offense. And NEVER feed or give something to drink to the patient. See #2 again.
If we ask you for a urine specimen, please get it to us as quickly as possible. We need it. We really do.
If there are other kids in your family that do not need to be at the ED if you are there, please try to find someone to come get them or take care of them before you come. You do not want your kid in the ED unless they are being seen as a patient. I understand extenuating circumstances happen, but this will make everything easier for everyone if extra kids aren’t there.
About the Author - Sarah K. Wells, MSN, RN, CEN, CNL is an educator, speaker, blogger and owner of New Thing Nurse, a professional and academic coaching company for the nursing world. New Thing Nurse is organized to provide support and guidance to aspiring nurses, newly graduated nurses, and veteran RNs looking to make a change in their life.
Whether it’s a new school, new job or new idea,
New Thing Nurse wants to help with your new thing!